What is an EHR workflow and why it matters ?
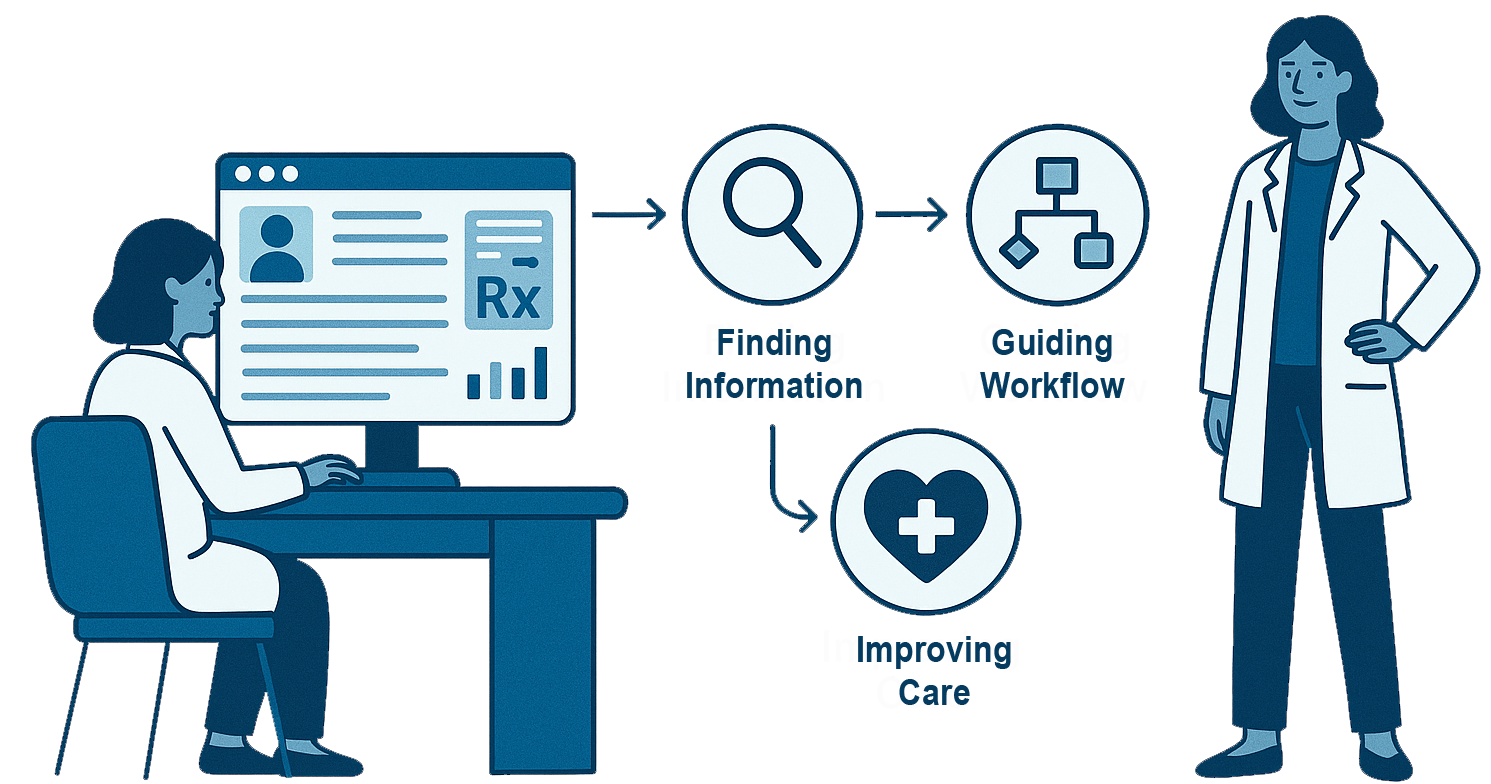
In today's fast-paced clinical environments, physicians and care teams rely heavily on electronic health records (EHRs) to access information, coordinate care, and support clinical decision-making. Yet many clinicians continue to face challenges navigating complex interfaces, locating essential patient data, or retrieving evidence-based guidance when they need it most. As healthcare systems expand and multidisciplinary teams grow, maintaining consistent, evidence-based care across departments has become both a priority and a persistent struggle.
As patient care becomes increasingly complex-often involving multiple specialties, multimorbidity, and frequent transitions between inpatient, outpatient, and specialty settings-clinicians face a substantial cognitive and coordination burden. The 2011 AHRQ report identified "Care Coordination" as one of its core quality-of-care priorities, highlighting that effective coordination across providers and settings remains a major challenge in U.S. healthcare. At the same time, clinicians must keep pace with continuously evolving clinical guidelines and best practices across numerous disease areas-a challenge for sustaining high-quality care in a fragmented, multispecialty environment. Collectively, these factors make it increasingly difficult to maintain shared situational awareness and ensure cohesive, patient-centred care across the continuum*1.
A 2024 scoping review showed that EHR-integrated digital technologies helped improve medication-related outcomes in hospitalized adults, possibly reducing adverse events and promoting safer care-when implemented with attention to equity and risk stratification.
In the same vein, design of the EHR interface matters: a 2025 systematic review found that poor EHR design contributes to usability problems-which can lead to medication errors, including overdoses.That means that a well-designed EHR not only supports evidence-based care, but also reduces safety risks.
A comprehensive 25-year review of EHRs and interoperability showed that EHR adoption improves care by strengthening information exchange, reducing duplication, and enabling real-time collaboration across disciplines*3.
Centralized, structured patient data:
- Supports smoother transitions between primary care, inpatient, outpatient, and specialty settings,
- Reduces fragmented or conflicting information,
- Allows clinicians to access a patient's full history quickly, and minimizes unnecessary tests and delays.
Interoperable EHRs also enhance patient safety by improving the accuracy and completeness of documentation-especially during handoffs and transitions of care. Integrated workflows have been shown to reduce clinician workload, improve efficiency, and support continuity by ensuring that every team member has access to the same, up-to-date information.
What are the main barriers to successful EHR implementation and long-term adoption ?
Successful EHR implementation and long-term adoption face several key barriers, spanning technical, organizational, and human factors. Major challenges include:
- Governance & Strategy Gaps: Lack of clear leadership or policy frameworks can fragment adoption.
- Infrastructure & Technical Limitations: Inadequate hardware, networks, or IT support hinder rollout, especially in smaller or resource-limited settings.
- Interoperability Issues: Poor data standardization and incompatible systems limit seamless information exchange.
- Human Resource & Training Constraints: Insufficient training, low digital literacy, and resistance to workflow changes reduce clinician adoption.
- Financial Constraints: High costs for software, maintenance, and customization can be prohibitive.
- Workflow & Usability Challenges: Poor interface design and misaligned workflows disrupt care delivery and increase cognitive burden.
Addressing these barriers requires coordinated leadership, adequate resources, standardized systems, effective training, and user-centred design to ensure sustainable, high-quality EHR use*4.
Why EHR-Driven Consistency Is the Path Forward ?
Healthcare delivery is increasingly team-based, distributed, and information-heavy. As a result, consistency-across departments, specialties, and roles-is more important than ever. EHRs, when designed and implemented well, serve as the backbone of this consistency*5.
They make it possible to:
- deliver the same high-quality, evidence-based care across all settings,
- reduce variability and close gaps in communication,
- support clinical reasoning with accurate and timely information,
- improve efficiency and reduce burnout, and
- enhance patient safety at every step of the clinical journey
Ultimately, EHR-driven workflows are not just digital checklists-they are foundational tools for improving healthcare quality, safety, and equity. By aligning information access, standardized processes, and evidence-based decision support, healthcare organizations can build a more coordinated, reliable, and patient-centred system.
- *1 Agency for Healthcare Research and Quality(2011). National Healthcare Quality and Disparities Report. Rockville, AHRQ. National Healthcare Disparities Report
- *2 Evaluating EHR-Integrated Digital Technologies for Medication-Related Outcomes and Health Equity in Hospitalised Adults: A Scoping Review (2024), Journal of Medical Systems.Evaluating EHR- Integrated Digital Technologies for Medication-Related Outcomes and Health Equity in Hospitalised Adults: A Scoping Review - PubMed
- *3 Shen Y, Yu J, Zhou J, Hu G (2025). Twenty-Five Years of Evolution and Hurdles in Electronic Health Records and Interoperability in Medical Research: Comprehensive Review. J Med Internet Res.Journal of Medical Internet Research - 25 Years of Electronic Health Record Implementation Processes: Scoping Review
- *4Dehghan M, Behzadi A, Mehrolhassani MH, Ghaemi M (2026). Challenges and facilitators of electronic health record implementation: a scoping review. International Journal of Medical Informatics. Challenges and facilitators of electronic health record implementation: a scoping review-ScienceDirect
- *5 Tsai C. H., Eghdam A., Davoody N., Wright G., Flowerday S., & Koch S. (2020). Effects of Electronic Health Record Implementation and Barriers to Adoption and Use: A Scoping Review and Qualitative Analysis of the Content. Life, 10(12), 327. Effects of Electronic Health Record Implementation and Barriers to Adoption and Use: A Scoping Review and Qualitative Analysis of the Content Comment